Background:
Diamond-Blackfan anemia (DBA) is a rare inherited bone marrow failure syndrome (IBMFS) marked by erythroid hypoplasia, reticulocytopenia and macrocytosis, and associated with congenital malformations and an increased risk of developing malignancies. From a clinical and molecular perspective this disease is highly heterogeneous, and no clear genotype-phenotype correlations can be found. Since the majority of molecular defects have been found in ribosomal protein (RP) genes, DBA is regarded a "ribosomopathy". While the molecular basis has been studied intensively, the pathophysiology of DBA is still not fully understood. One of the major unresolved issues is how RP gene mutations result in the specific erythroid defect seen in DBA, with macrocytic erythrocytes and increased adenosine deaminase activity. In addition, the highly heterogeneous and variable clinical presentation and disease course, even in patients with similar molecular defects, remains enigmatic. Hence, in order to investigate the cellular defect, and increase our understanding of disease pathophysiology and clinical heterogeneity, novel tools are needed. In this study, we explore the potential of untargeted metabolomics on dried blood spots and report for the first time a metabolic fingerprint for DBA.
Aims:
Defining a metabolic signature for DBA in order to: 1. Increase our understanding of cellular determinants of impaired ribosome biogenesis, and 2. Extend the toolbox for diagnostic evaluation.
Methods:
Untargeted metabolic profiling was performed on DBS samples obtained from 18 DBA patients and 45 healthy controls using direct infusion high resolution mass spectrometry following a previously established approach1. Statistical analysis was performed in MetaboAnalyst and predictive modeling was executed within R-software.
Results:
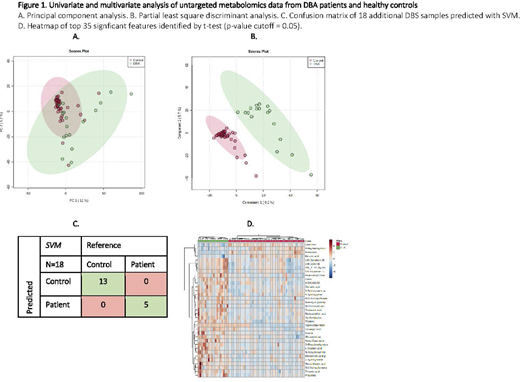
In total, 1917 unique metabolite features were identified in DBS samples from patients and controls. Multivariate analysis yielded distinct metabolic profiles, reflected by natural separation detected by principal component analysis (Figure 1A), and emphasized by clear distinction with partial least square discriminant analysis (Figure 1B). This 'metabolic fingerprint' was incorporated into a machine learning algorithm, and subsequently a binary classification (or prediction) model was constructed by randomly dividing patient and controls into 'training' (32 HC, 13 DBA) or 'test' set (13 HC, 5 DBA). Accurate class assignment was achieved for all patients and controls in the training set (Figure 1C). Prominent metabolites in the fingerprint and classification algorithm were a.o. menadione (a vitamin K precursor), 4-hydroxyproline (collagen component) and methylmalonylcarnitine (an acylcarnitine). In addition a large number of interesting metabolites were identified that could provide novel starting points for studying/understanding downstream effects of RP defects in DBA and therapeutic mechanisms (Figure 1D).
Conclusion:
In this study we performed untargeted metabolomics on dried blood spots from a substantial cohort of DBA patients and report for the first time a metabolic fingerprint of this disease. By incorporating this fingerprint in a machine learning algorithm we underlined the diagnostic potential of this approach. Moreover, the metabolites identified in this fingerprint, provide promising starting points for further studies to increase our insights in disease pathophysiology, including the mechanism involved in elevated eADA activity, as well as the development of new therapeutic strategies.
References:
1. de Sain-van der Velden MGM, van der Ham M, Gerrits J, et al. Quantification of metabolites in dried blood spots by direct infusion high resolution mass spectrometry. Anal Chim Acta. 2017;979:45-50.
Wijk:Agios Pharmaceuticals Inc.: Research Funding; RR mechatronics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal